Well, we did it. We made it through 2020, a year no one could have ever expected. A year that we were all “safer at home” and “socially distanced.” A year in which we all struggled as a collective against a common enemy and were challenged on a personal level as well.
It’s easy to look back on this as a very difficult year, but for me it was also a year of major growth, learning, and finding love. Love for myself, my partner, my family and friends, and even for strangers. A year to prioritize my health, both physically and mentally. A year to allow many tears and also to find joy in the most ordinary of days.
I’m actually unable to hold back tears thinking of all we went through this year with such little reprieve. To go through cancer on top of it all was just ridiculous, honestly. So, I am grateful to sit here and reflect on the highs and lows of 2020. I am even more grateful to be able to look ahead to the ordinary joys, the eventual hugs, and the lessons that 2021 will bring.
I know I’ve mentioned this before, but on my 30th birthday last year, I kept feeling that 2020 would be a big year. Not like the “best year ever” kind of year, but the kind where you’re challenged in all the important ways. I usually decide on a word that symbolizes my intentions for the year, and I just couldn’t pick one last year, but as the second quarter of the year began with COVID and a cancer diagnosis, I found myself always coming back to a Japanese phrase I learned a few years ago:
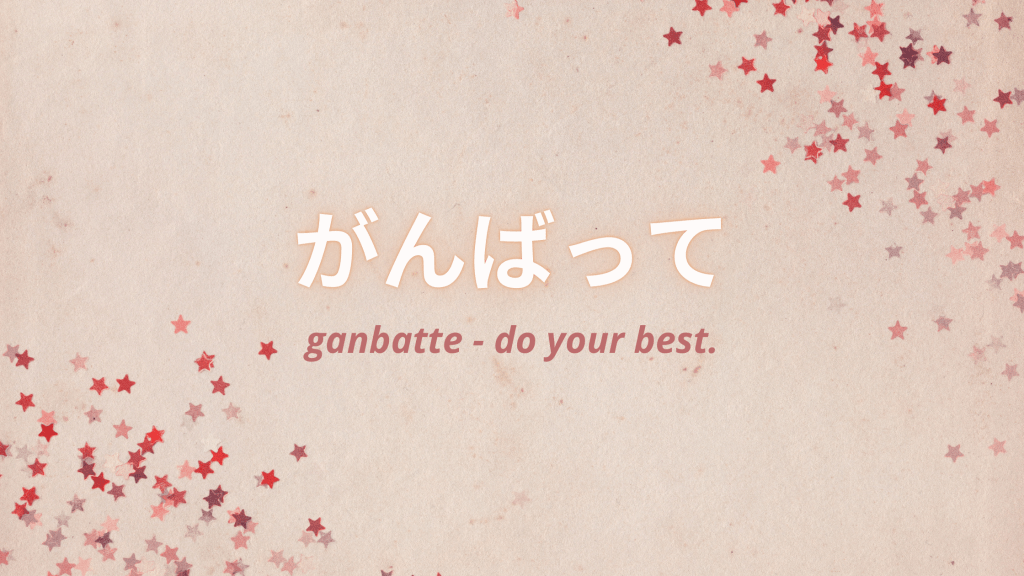
And so that’s what I’ve done this year. I just kept putting one foot in front of the other and doing the best I could to get through each day. Trust me, some days were better than others and there were many days that I had to ask for help. So to those of you who prayed for me, who let me cry with you on the phone, who laughed with me on zoom calls, who sent cards and letters, who wore masks & socially distanced to protect the immunocompromised – I am incredibly thankful for you.
A few highlights from this year:
Getting to spend a whole month with my mom in Hawaii. Staycations. Cooking at home and learning new recipes. Being outside more often. Meeting new people (mainly my excellent medical team and an incredible group of cancer thrivers). Growing closer to my husband as we rounded out our second year of marriage and head into our third. Working on my Pilates certification. New babies. Friends getting married. Learning my own strength.
I won’t dwell on the lows, but I will remember how much I learned from them. This year my word is JOY. I hope to find more joy in each day, be more present, and celebrate every little victory. There will be setbacks, I’m sure of it, but if I’ve learned anything this year, it’s that they can be overcome. Wishing you all a happy, healthy, safe new year and sending you so much love and gratitude.
Cheers to 2021! ❤