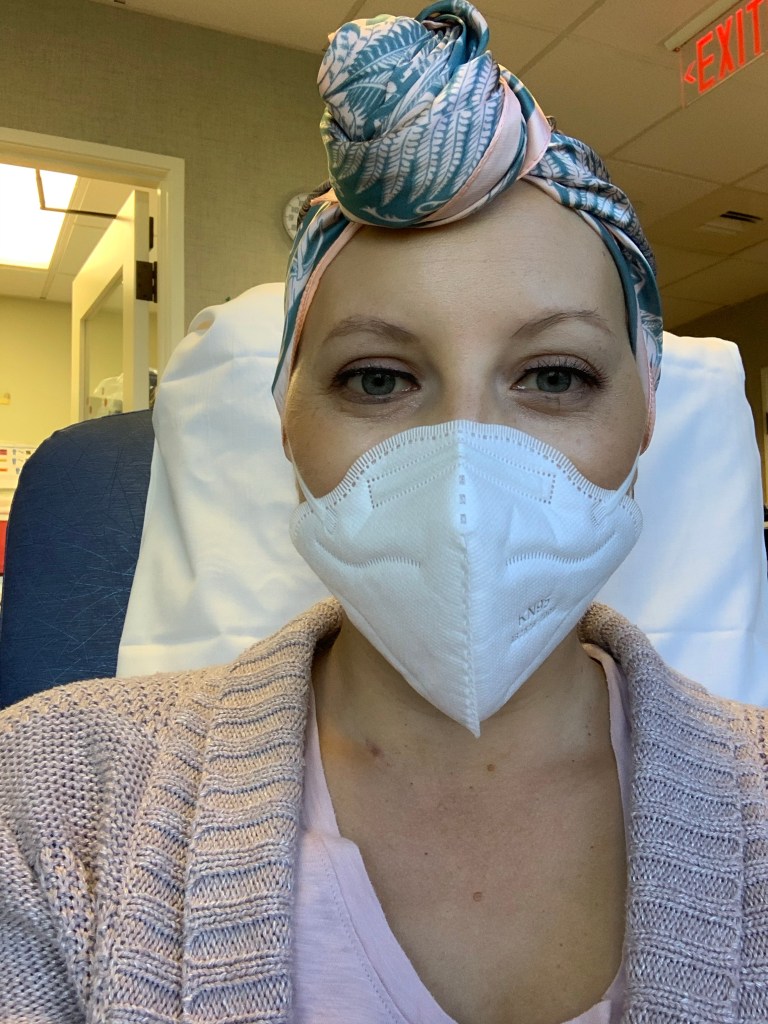
Celebrating with tears of joy today after finishing my last chemo yesterday. 16 rounds over 20 weeks. Conquering the Red Devil and getting through taxol without neuropathy are major victories, and I’m feeling so relieved to be DONE! I could not have done it without all of your support.
There’s still more treatment ahead, but I’m feeling I can manage anything now that chemo is behind me. I am so grateful to God and for all of the love of my family and friends and this great little breast cancer community I’ve found on Instagram that have gotten me through the past 5 months.

I will still receive two GCSF injections to boost my white blood cells this week as my oncologist doesn’t want me too immunocompromised in this COVID life we’re all living in. Then, I’ll re-test my labs in two weeks including a thyroid panel and vitamin D screen that I asked for. My oncologist has been really great about letting me lead my care to some extent and not just telling me what we’re going to do each week. Honestly, I wish every doctor were like that. I am so grateful for her and my whole team of docs who’ve listened to my concerns and took action immediately throughout this whole process.
Next week, I am scheduled to repeat my breast ultrasound, mammogram, and MRI to see where I’m at post-chemo. I am still unable to feel the tumor, but that doesn’t mean I don’t still have a bit of “scanxiety” about the slight possibility that there’s still something there or that the tumor will grow again being off chemo for several weeks before surgery. Please send prayers for good results!

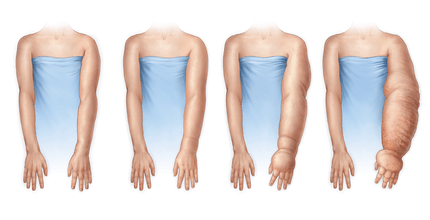
I’ll meet with my surgeon on November 9, and will hopefully be able to get in for surgery before Thanksgiving. I’m still leaning toward breast-conserving surgery (a lumpectomy) which means I’ll do radiation for several weeks after recovering from surgery. I’ve done a lot of research on different types of surgeries and, besides my intuition telling me not to go for the more aggressive approaches, the research actually backs me up on that decision. For women with similar early-stage cancer to mine, the 5-year survival rate is 94.3% for breast-conserving surgery, 93.3% for mastectomy alone, and 83.7% for mastectomy with radiation.1
I am also biased in that I know that recovery from a mastectomy is really challenging and the complications can be much greater. To have further breast reconstruction on top of that would take multiple surgeries, and honestly, I’m just ready to move on from cancer in so many ways. I know it will always be a part of me, but treatment can end sooner than later if I go this route!

For now, I’m going to rest and celebrate being done with the hardest part of this little bump in the road. My mom will finally be down to visit in a few weeks and I’m looking forward to that! I wrote down a few things I want to remember from this experience so far and I’ll share a few of them with you here:
- Faith in God is all you need to conquer anything.
- The people you love are the most important thing in your life – tell them you love them often and mean it.
- Find the immense joy in your daily life – there’s no need to search far and wide for it.
- Spend time in nature – in quiet, being active, barefoot if you can.
- Know and trust your body. Know that it’s strong and demands to be respected and understood.
Learning you have breast cancer at age 30 isn’t in anyone’s plans for life, and being diagnosed with one of the most aggressive forms of breast cancer doesn’t make it any easier. I want to remind you all that if you think something is off with your body, get it checked out. Don’t take no for an answer from your doctor. You’re not “too young.” You’re not overreacting. YOU are the only one that knows your body well enough to decide if something is off.
I love you all. Thank you for being with me on this ride.
Aloha ❤