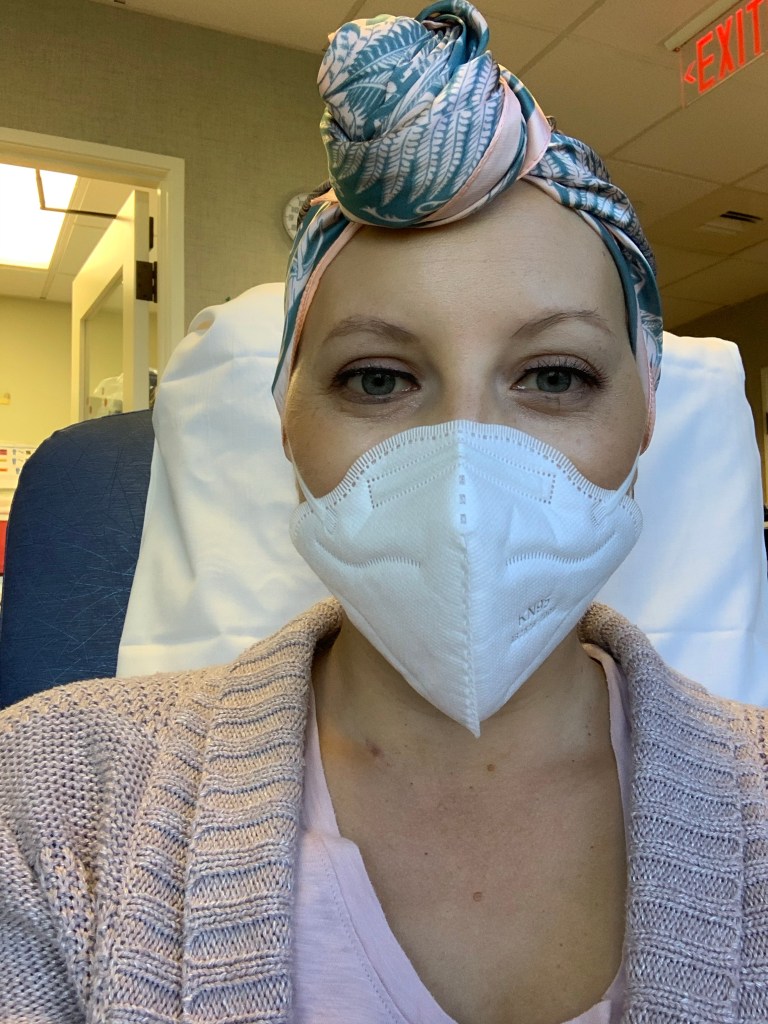
Well, another week or so has passed! I had my 12th (8th taxol) treatment last Thursday and that means I’m 3/4 of the way through chemo. I am getting ahead of myself a little bit with the countdown and keep finding myself saying things like “only 3 left after this week,” but who can blame me?
By the time I’m done with chemo at the end of October, I’ll have been in treatment for a full 5 months. Everything goes fast and slow at the same time. I’m going a little bit stir crazy working from home, working out at home, getting most of my social interaction from home (thanks, FaceTime & Zoom) as I know most of you are, too. I’m thankful we’re starting to re-open beaches, trails and business this week so I’ll have some more opportunity to get out of my dang apartment! Island fever is a real thing, and I’m really looking forward to travelling again when my health and the COVID situation is more stable.
For the past few weeks I’ve been having some rib pain on my left side. My physical therapist brain feels that it’s postural from sitting so much, but my cancer patient brain tells me to be more cautious as it could be one of several other things including bone pain from my zarxio injections, a rib fracture (although I didn’t specifically injure my ribs, all the weekly steroids and injections do put me at risk for lower bone density), or, in absolute worst case scenario, a metastasis to my ribs. My oncology APRN and I agreed to monitor it and if pain becomes worse we’ll do a new scan. It’s getting better with stretching and doing more standing or lying flat so I think all is going to be okay.
FYI – “cancer pain” (pain from a tumor or metastasis) typically follows a unique pattern. Often, pain is worst at night or will wake you up in the middle of the night (for some people, it wakes them at the same time every night). Cancer pain is not resolved with changing your position or stretching typically. Over time, cancer pain usually becomes consistent or unrelenting. Anyone with active cancer or a history of cancer should be aware of pain anywhere in their body and consult their doctor as soon as possible if the pain follows any of these patterns. You can see my other post here about cancer warning signs for other symptoms that might accompany pain.

Also, in the past few weeks I’ve been diving a little deeper into the Native Hawaiian practice of Ho’oponopono which translates to “to make right twice (with self & others).” I stumbled upon this after doing a tapping meditation based on Louise Hay’s work. Louise believed that cancer can be related to a deep resentment held in the body and she suggests healing your relationships with others as part of a cancer journey.
Ho’oponopono is the ancient Hawaiian way of resolving conflict and issues within a family but also applies to government or individual relationships. It is the process of forgiveness and making right relationships that have gone wrong. The process of Ho’oponopono can be done with a mediator who is the go-between for the two individuals or parties, but it can also be done individually with mindfulness and meditation on the relationship.
As part of my tapping and meditation, I’ve been using the common Ho’oponopono meditation which is as follows:
I’m sorry.
Please forgive me.
Thank you.
I love you.
I envision the person with whom my relationship requires healing as I’m meditating. This process has been very freeing and beautiful to me. I urge you to try it and to read this article and this article to learn more if you’re interested. Having cancer has put me on a journey to learn more about myself and I think Ho’oponopono is one of the most healing practices I’ve learned so far.
On a fun note, my hair is slowly starting to grow back in, although it’s only baby hairs. At the same time, my eyebrows and lashes are pretty much gone now. I’m looking forward to all of that renewal post-chemo, too! Hope you all are having a great week! I’m looking forward to posting a lot more PT and breast cancer content in October as it’s both National Physical Therapy Month and Breast Cancer Awareness Month so STAY TUNED!!
Aloha ❤