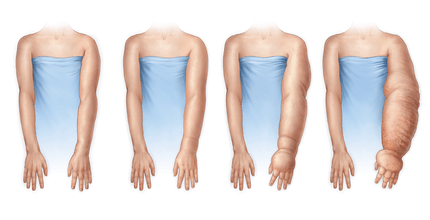
Lymphedema, a type of swelling in the arm, is an unfortunate complication after breast cancer surgery. I hope this blog will give you a better understanding of the lymphatic system and how to recognize early signs of lymphedema if you’ve recently had or are about to have breast cancer surgery.
*Technically, lymphedema can occur in any limb after lymph nodes are removed, but to keep it simple, I’ll focus on upper extremity lymphedema today.
Overview of Lymphatic System
The lymphatic system is a network of nodes, vessels and organs that function as the body’s immune system. Lymphatic fluid (or lymph) is a protein-rich fluid which contains white blood cells. Lymph carries bacteria and viruses to be filtered through the lymph nodes and helps to prevent infection in the body.
Unlike blood, which is circulated around the body, lymph only flows one way (toward the heart) and requires a pressure gradient and muscular contractions to flow efficiently.
Photo borrowed from Merck Manual1
Lymphatic Disruption after Breast Surgery
From my last post, you know that surgery for breast cancer usually involves removal of the tumor itself as well as removal of lymph nodes in the axilla (underarm). Lymph node removal is done because cancer cells can break off and travel through the lymphatic system and those nodes in the axilla are usually the first place they go.
To be sure the correct nodes are examined, the surgeon uses a radioactive dye to determine which nodes drain directly from the tumor site. Procedures to remove lymph nodes can range from removal of only a few nodes in a sentinel lymph node biopsy to many nodes (up to 20 nodes) in an axillary dissection.
With any amount of nodes removed (but especially with >5 nodes removed), there can be disruption to lymphatic flow through the axilla. In some cases, the lymph is unable to drain from the arm, resulting in lymphedema.
Lymphedema presents as a “swollen” arm, but this is not your usual swelling for two reasons. One, because lymphatic flow is a one-way street, the extra fluid needs to be physically cleared in some way (more on this in a minute…) and, two, because lymph is full of protein and fats that won’t drain into the venous system the way typical swelling does. The limb can actually grow and harden if left untreated.
Studies show that lymphedema occurs in 0-3% of people who choose lumpectomy and up to 65-70% of those who have a modified radical mastectomy.3 Radiation therapy also seems to increase the risk of lymphedema. While many people will develop symptoms in the first 3 years after surgery, lymphedema can take up to 5 years to develop after cancer treatments. Be sure to ask your doctor or physical therapist what your risk for developing lymphedema is and learn about risk reduction practices.
Signs & Symptoms of Lymphedema
- Swelling in the arm (usually only on side of surgery)
- Heaviness/tightness of the arm
- Reduced range of motion of the joints in the affected arm
- Thickening/hardening of the skin
Physical Therapy Treatment for Lymphedema
A trained lymphedema physical therapist can be an incredible asset to someone who develops lymphedema. Ideally, a physical therapist will be able to work with a patient pre- and post-operatively to monitor girth measurements of the limb and identify lymphedema early on. Stage I lymphedema is potentially reversible, and both stage II and III can demonstrate significant reduction, so seeing a PT sooner than later is key in managing this condition!
With development of lymphedema, a physical therapist can perform or recommend the following interventions:
- Bandaging of the limb or prescription of compression garments
- Manual Lymphatic Drainage (specialized lymphatic massage)
- Exercise prescription (progressive muscle pump, aerobic activity)
- Patient education on proper skin care and prevention of infection
It’s important to see your doctor or physical therapist as soon as possible if you notice signs/symptoms of lymphedema. Here is a great resource to find a lymphedema specialist in your area. As always, feel free to reach out to me with any questions!
Aloha ❤
Big thanks to Joanne Zazzera, PT, DPT, WCS, for sharing her knowledge and editing this blog!